Addiction is a complex, chronic condition that affects the brain, behavior, and overall well-being of an individual. One of the most challenging aspects of addiction is the recurring cycle of substance use, temporary abstinence, and relapse. Many people struggling with addiction find themselves “chasing the high”—seeking the intense euphoria that comes with drug or alcohol use, even after experiencing serious consequences. Understanding this cycle is key to supporting recovery and preventing relapse.
The First High and the Hook
Addiction often begins with experimentation or recreational use. The first time someone uses a substance, especially powerful drugs like opioids, meth, or cocaine, they may experience a surge of pleasure due to a massive release of dopamine in the brain. This feeling of euphoria creates a powerful memory that the brain registers as something worth repeating.
Over time, the brain adapts to the presence of the substance, producing less dopamine naturally. This means the person needs more of the substance to achieve the same high—a phenomenon known as tolerance. Eventually, using becomes less about feeling good and more about avoiding the painful symptoms of withdrawal.
Dependency and the Need to Escape
As substance use becomes more frequent, physical and psychological dependence set in. The brain and body begin to rely on the substance to function normally. At this stage, addiction is no longer a choice; it becomes a compulsive behavior driven by cravings, emotional distress, and a need to escape reality.
Many people use substances to cope with trauma, anxiety, depression, or overwhelming stress. Unfortunately, the relief is only temporary, and the problems they are trying to escape often worsen with continued use.
The Illusion of Control and the Struggle to Quit
Even when someone acknowledges they have a problem, breaking free from addiction is incredibly difficult. They may try to quit “cold turkey” or reduce their use, but cravings, withdrawal symptoms, and emotional triggers can quickly lead them back to the substance.
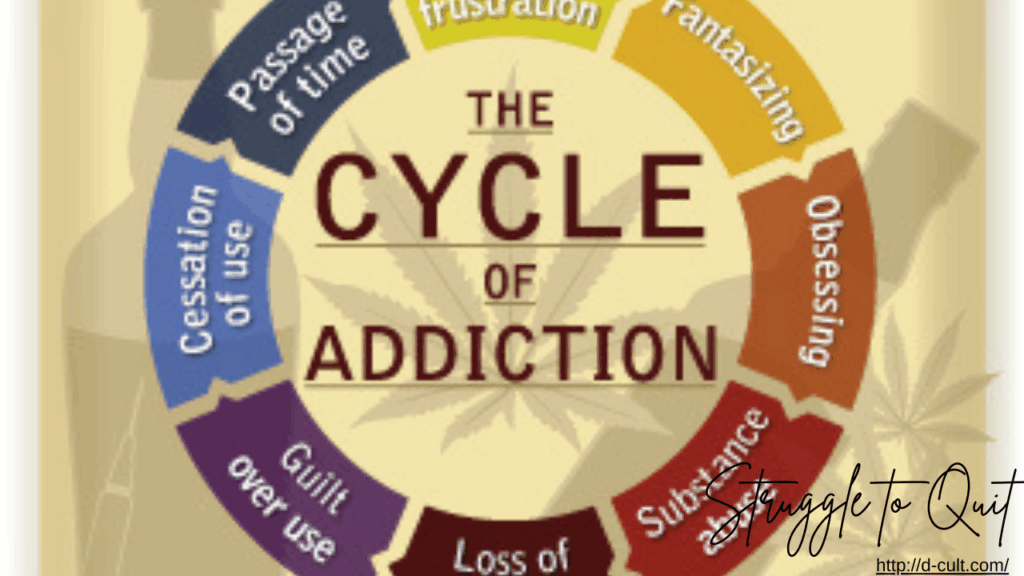
This creates a cycle of quitting and relapsing. After a period of sobriety, the individual may start to believe they can control their use or “just have one.” But the brain, still wired for addiction, often reacts by quickly returning to old patterns—sometimes worse than before.
The Role of Triggers and Relapse
Relapse is a common part of the recovery journey and doesn’t mean failure. Many factors can trigger a relapse: stress, exposure to people or environments linked to past use, negative emotions, or even positive events that the person associates with celebrating using drugs or alcohol.
Understanding these triggers and developing strategies to manage them is essential for long-term recovery. Counseling, therapy, support groups, and medication-assisted treatment can all help individuals regain control and reduce the risk of relapse.
Hope and Healing
Though addiction is a powerful force, recovery is possible. By understanding the biological and psychological aspects of addiction, we can move away from judgment and toward compassion. Recovery is not a straight path—it involves setbacks and learning experiences. With the right support, individuals can break free from the cycle of chasing the high and build a life rooted in stability, healing, and hope.
